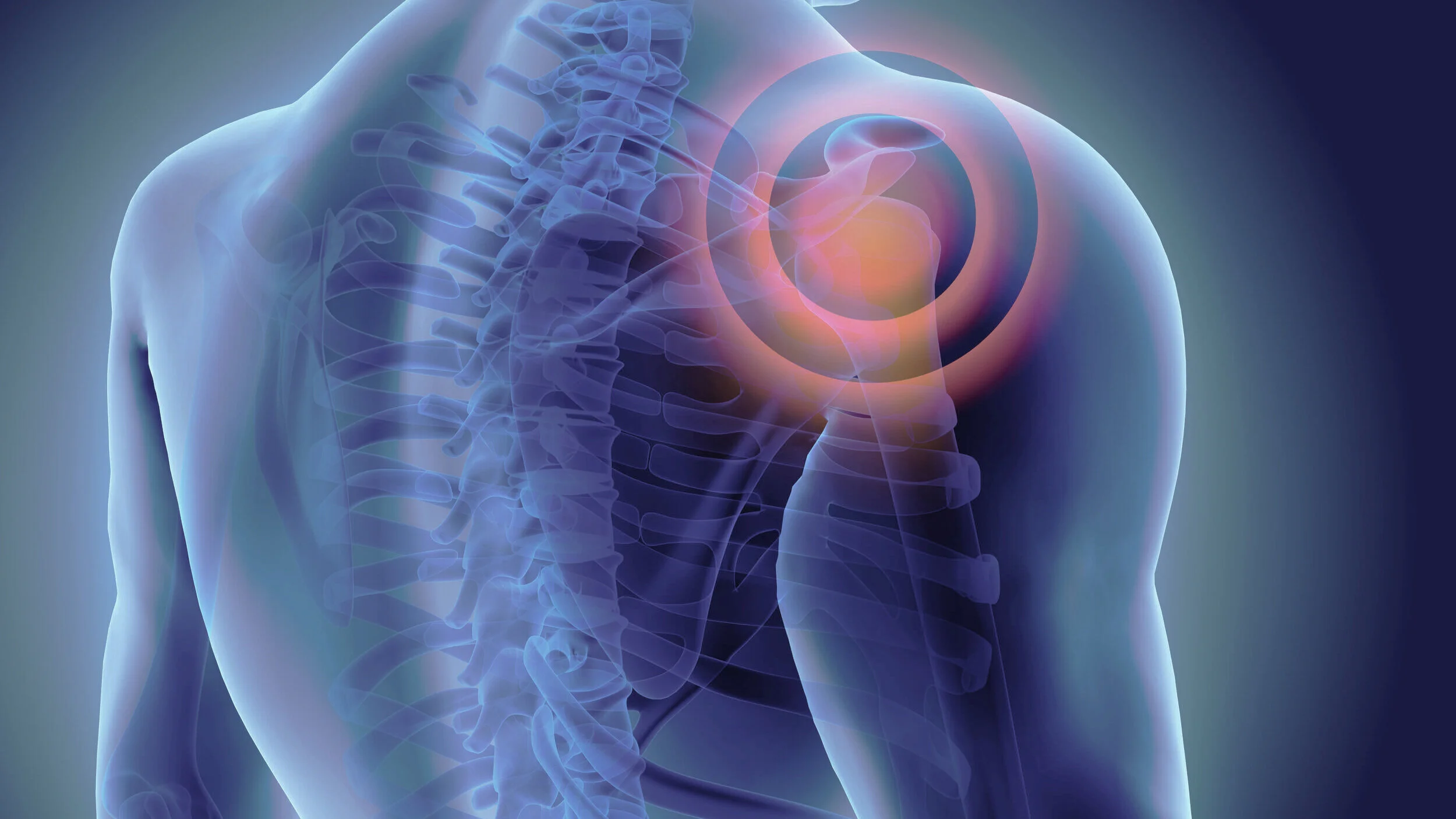
Frozen Shoulder.
The shoulder has a capsule that surrounds the ball and socket joint which is usually stretchy to allow for a large range of movement. Frozen shoulder (also known as adhesive capsulitis) is inflammation and tightening of the capsule which causes stiffness and severe pain in the early stages.
What causes a frozen shoulder?
Research is inconclusive as to the cause of frozen shoulder; it is a common condition, which will affect about 3% of adults at some stage in their lives. It is most common in people aged between 40 and 65 years. It is more common in people who have diabetes, an overactive thyroid, high cholesterol, a high body mass index, heart disease or a history of trauma. It can start after an injury but often starts for no reason at all.
A frozen shoulder typically progresses through three phases:
Freezing phase is usually extremely painful, especially at night. This phase can last anywhere from 2 to 9 months.
Frozen phase is where pain gradually eases but stiffness and limitation in movement remains and in some cases worsens. All movements of your shoulder can be affected. This phase can last anywhere from 4 to 12 months.
Thawing phase is where the pain and stiffness gradually settle and movement gradually returns to normal, or near normal. This phase can last anywhere from 1 to 3 years.
The time taken to progress through these phases is highly variable from person to person. Untreated, on average the symptoms last from 2 to 4 years, with some cases lasting less than this. Some stiffness remains, although most people regain enough movement to carry out everyday activities.
How is frozen shoulder diagnosed?
Usually Mr Moverley can diagnose frozen shoulder with a combination of clinical examination and a careful assessment of your symptoms.
As frozen shoulder can be confused with other conditions such as shoulder arthritis, further diagnostic tests are used for confirmation and to plan treatment:
X-rays can obtained on the day of your consultation they are frequently normal in frozen shoulder and that is useful, because it rules out shoulder arthritis as a cause for your symptoms.
MRI is not always needed but can be used to look for other conditions, such as a rotator cuff tear
Treatment options
Frozen shoulder is described as a 'self-limiting' condition. This means it will generally get better by itself, however because of the severity of symptoms patients often require treatment to expedite the recovery.
Non-operative Management
Non-operative treatment should always be exhausted before considering any form of surgery. Possible non-operative options include:
Rest, activity modification, and simple pain relief can provide good benefit, particularly in the early stages of the disease.
A focused physiotherapy program to stretch the soft tissues of the shoulder to regain range of motion.
Steroid injections are often used to provide short-term pain relief and reduce inflammation, which can then allow you to participate in physiotherapy. Ideally these injections are given using an ultrasound to guide the needle into the ball and socket joint. 80% of patients will improve after a single injection
Hydro-dilatation injection is similar to a steroid injection but uses a larger volume of fluid to stretch and burst the shoulder joint capsule. Patients can find this procedure painful but it is effective in approximately 90% of patients.
Surgical Management
Shoulder Arthroscopy
The operation for frozen shoulder is called an arthroscopic (key-hole) capsular release.
The operation involves release of the inflamed and contracted capsule around the ball and socket followed by gentle manipulation of the joint to stretch the released tissue.